Dean’s Day 2023
The Ulrich Award honors outstanding students from the school’s professional-degree programs committed to serving the needs of disadvantaged communities. The award is open to all Dean’s Day projects that show a commitment to the public health service and the underserved.
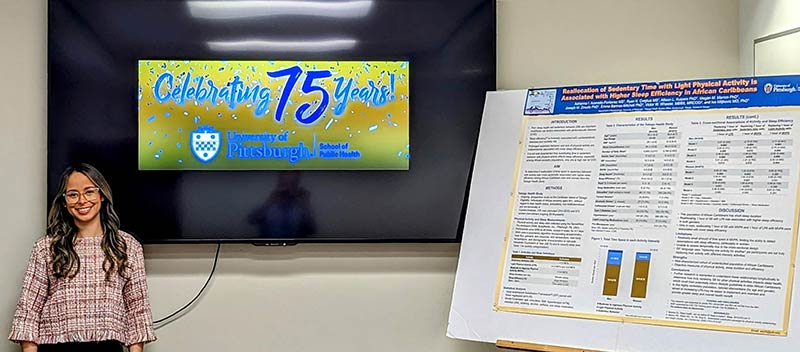
EPIDEM
“Reallocation of Sedentary Time with Light Physical Activity is Associated with Higher Sleep Efficiency in African Caribbeans”
Adrianna I. Acevedo-Fontanez , Ryan K. Cvejkus , Marquis Hawkins, Allison L. Kuipers, Megan M. Marron, Joseph M. Zmuda, Emma Barinas-Mitchell, Victor W. Wheeler, and Iva Miljkovic
Introduction: Sleep efficiency (or sleep continuity, i.e., a ratio of time spent sleeping to time spent in bed), is inversely associated with hypertension, impaired glucose metabolism, CVD risk, and mortality risk. Prolonged sedentary behavior and physical activity are independently associated with sleep efficiency. However, it is not well documented how substituting time in sedentary behavior with physical activity affects sleep efficiency, especially among African-ancestry populations, who are at high risk for CVD.
Aim: To determine if displacement of sedentary time with activity was cross-sectionally associated with higher sleep efficiency among African Caribbean men (n=235) and women (n=673) from the Tobago Health Study.
Methods: Sleep efficiency, sedentary behavior (SB), light physical activity (LPA), and moderate to vigorous physical activity (MVPA) were collected using a SenseWear Pro Armband. Participants wore the armband at all times, except in water, for 4-7 days. We used the Isotemporal Substitution Framework paired with linear regression to examine associations of SB, LPA and MVPA with sleep efficiency adjusting for age, education, BMI, hypertension, diabetes, smoking, alcohol consumption, caffeine intake, and sleep medication.
Results: Men (mean age ± Standard deviation: 63.2 ± 8.2 years; mean BMI 28.2 ± 4.8 kg/m2) spent on average less time in SB (12.4 ± 2.9 hours/day) and more time in LPA (4.7 ± 2.1 hours /day) and MVPA (0.92 ± 0.88 hours/day) than women (mean age 55.6 ± 8.7 years; mean BMI 31.8 ± 6.4 kg/m2) (all p-vales <0.001). Men had lower sleep efficiency (74.6% ± 10.4) than women (81.2% ± 0.96; p-value <0.001). Cross-sectionally reallocating 1 hour of SB with LPA was associated with a 1% higher sleep efficiency (p-value=0.013) in men and with a 0.38% higher sleep efficiency in women (p-value=0.065). In men, reallocating 1 hour of SB with MVPA and 1 hour of LPA with MVPA were significantly associated with lower sleep efficiency [-1.9% (p-value=0.013) and -2.8% (p-value=0.004), respectively]; in women these associations were not statistically significant. Interaction term for sex and sleep efficiency was statistically significant (p-value <0.0001).
Conclusions: In this population with short sleep duration, reallocating 1 hour of SB with LPA was associated with higher sleep efficiency in both genders. In contrast, among men only, reallocating 1 hour of SB to MVPA and 1 hour of LPA to MVPA were unexpectedly associated with lower sleep efficiency. Further research is warranted to understand these relationships longitudinally to determine how truly replacing SB for activities of different intensities impacts sleep health, which could then potentially inform lifestyle guidelines in older Caribbeans. In this highly sedentary population, interventions aimed at increasing LPA may be easier to implement and maintain and provide greater sleep and overall health benefit.